Since May, there have been a lot of stories in the news about monkeypox. Depending on which stories you read, you may have heard that it’s not very contagious, or that it’s very contagious. You may have heard that it’s not very dangerous, or that it’s very dangerous. It’s confusing. But we can help.
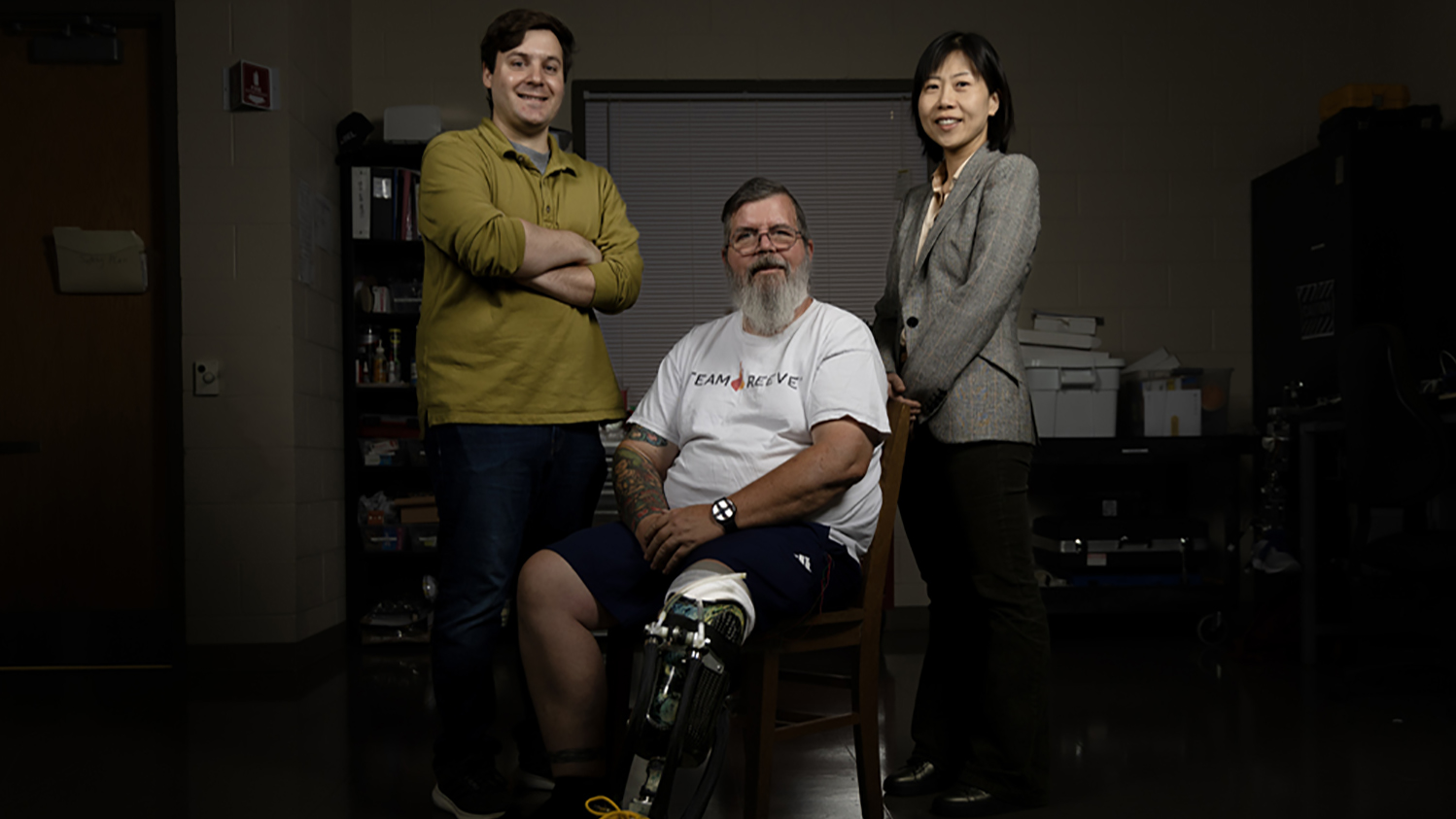
To help get a handle on what we know about monkeypox, we spoke with Julie Swann and Matt Koci. Swann is a systems engineer with expertise in public health whose work focuses on making health care more efficient, effective and equitable. Swann is the department head and A. Doug Allison Distinguished Professor of the Fitts Department of Industrial and Systems Engineering at NC State. Koci is a virologist and immunologist whose work focuses on host-microbe interactions; he is a professor in NC State’s Prestage Department of Poultry Science.
The Abstract: So, first question: what is monkeypox?
Matt Koci: Monkeypox is a virus. It belongs to a family of viruses known as the pox family which contains the smallpox virus, camelpox and cowpox viruses, just to name a few of its close relatives.
However, because names in science don’t always make sense, chickenpox isn’t a pox virus. Keeping with that theme, while monkeypox is a pox virus, it should probably be called rodentpox, since they are the more common carrier of the virus.
This isn’t like SARS-CoV-2. Monkeypox isn’t a new virus. We’ve actually known about this virus since 1970. There have been several outbreaks of monkeypox over the past 50 years. Most have occurred in western Africa, but we’ve seen several outbreaks around the world. Most of these start off with someone who recently returned from a trip to Africa. One major exception to this pattern was a 2003 outbreak here in the U.S. that ended up affecting 71 people. The culprit in this case was an infected prairie dog that was purchased as a pet. It was later discovered that the prairie dog got it from Gambian pouched rats imported by an exotic-animals dealer.
But while this isn’t a new disease, something is different this time. This current outbreak has spread to over 76 countries, infected over 19,000 people, and lasted longer than any other previous outbreak. Right now, we don’t know why that is, but early evidence suggests the variant of monkeypox associated with this current outbreak has evolved to spread from person-to-person more efficiently than we’ve ever seen monkeypox do before.
Julie Swann: I agree with all of that. The summary is that monkeypox is a virus that has jumped from animal hosts to humans, and it is now spreading between or among humans independently. The current outbreak is human-driven and not related to monkeys or other animals. In the coming years, we will likely continue to hear about diseases that gain the ability to make human-human transmission and spread in new ways or to new populations. Monkeypox is not as easily spread as the virus that causes COVID-19, although the number of new cases and new geographical locations is staggering.
TA: How hazardous is monkeypox to human health? Is it fatal? Does it leave scars?
Koci: There are a lot of diseases that are worse than monkeypox. From a public health perspective COVID-19 is still a much bigger issue, but that doesn’t mean we can ignore monkeypox. While monkeypox disease typically clears on its own in about 2 to 4 weeks, it’s going to put painful blisters in places the sun don’t shine for days to weeks. More severe illnesses that require hospitalization can happen, especially in kids and the immunocompromised. Looking at previous outbreaks, case fatality rates have been as high as 3-6%, but so far during this outbreak while there have been a few deaths globally, the case fatality rate is well under 0.1%, and none have been reported in the U.S.
If you’ve been infected, symptoms typically start between five and 13 days later, but could be as long as three weeks later. Recent data from the current outbreak in the U.S. suggest the three most common first symptoms people report experiencing is fever (41% reported fever as the first symptom), rash (41%), or chills (16%). Regardless of what the initial symptoms were, patients reported several symptoms, some more common than others: rash (100% reported experiencing a rash at some point during the their illness), fever (63%), chills (59%), lymphadenopathy (swollen lymph nodes, 59%), malaise (general discomfort, 57%), myalgia (muscle aches and pains, 55%), headache (51%), rectal pain (22%), pus or blood in stools (21%), abdominal pain (12%), rectal bleeding (10%), tenesmus (feeling like you have to go #2, but there’s no #2 to go, 10%), vomiting or nausea (9%).
The one symptom that everyone seems to experience is the tell-tale rash and blisters. These have been reported all over the body: genitals (46% reported experiencing a rash and/or blisters here), arms (40%), face (38%), legs (37%), perianal (between the buttocks and around the rectum, 31%), lips and mouth (25%), palms of hands (22%), trunk (22%), neck (18%), head (14%), soles of feet (11%). This normally clears up after 2-4 weeks; however, more severe cases requiring hospitalization can occur, especially in young children and the immune compromised. The rash and blisters can be quite painful, and can lead to scarring after they clear up.
Swann: Previously, monkeypox has had two genetic groups (or “clades”). The group in the Congo Basin in central Africa has had higher fatality rates (e.g., sometimes 10%), while the group in west Africa has had lower rates (e.g., 1%). So far, the variants that are circulating in the U.S. have had even lower fatality rates although there have been deaths. A number of patients are reporting significant pain, and the symptoms can last for weeks.
One of the concerns is not only the individual cases and outcomes that we are seeing, but also the possibility that the disease will become endemic in broad, new areas of the world. This possibility becomes more and more likely the slower the response to contain it.
TA: How contagious is monkeypox?
Koci: The good news here, at least historically, is that monkeypox doesn’t spread as well as smallpox did, and it certainly spreads a lot slower than COVID-19. However, I say historically because while we’ve had outbreaks of monkeypox in the past, those outbreaks have burned out after a few days, with very limited human-to-human spread.
This outbreak clearly has more human-to-human spread than we’ve seen in the past, so it’s not clear how much we can use past outbreaks as a guide. However, it still looks like direct contact with infected people (skin-to-skin contact) or with anything they may have recently touched is probably the most efficient means of transmission. But the virus is also likely in respiratory droplets as well, so following the 3 Ws we practiced for COVID-19 will go a long way to protect you. [Editor’s note: the “3 Ws” are: wear a mask, wash your hands and watch your distance – i.e., try to stay six feet away from others.]
Swann: It is less contagious than COVID-19 or influenza. In the past, monkeypox outbreaks have fizzled out before spreading widely. The current outbreak is different, possibly because of a combination of factors. There was likely monkeypox that had been undetected previously, there were amplifying events where the virus reached new people, and this was followed by global travel that spread it to new locations.
In general, I think of it as a disease that is spread through intimate contact. This could be skin-to-skin contact, prolonged kissing, sharing of towels, etc. Risk is higher for people who have multiple sexual partners, and it may be higher if someone has other conditions with rashes or lesions in the genital area.
We are also continuing to gather data on situations where transmission can occur in case the virus finds new pathways. There have been a small number of cases where transmission occurred within a household such as in people who used common clothing or bedding.
TA: I’ve also seen people claiming that monkeypox is only a sexually-transmitted disease. That’s not right, is it?
Koci: No. Well, historically, no. Monkeypox outbreaks generally start with an initial transmission from an infected animal to a person through some sort of bite or direct contact with the body fluids of the infected animal. From there spread from person-to-person happens through close contact with respiratory droplets, contact with the rash and/or blisters of an infected person, or even through direct contact with an object the infected person contaminated, like bedding, linens, or clothing.
Transmission has been associated with sex, but calling it a sexually-transmitted disease I think gives the wrong impression. Being in close contact, especially direct skin-to-skin contact, or contact with body fluids of someone with monkeypox is the best way to get it. So, can monkeypox be transmitted through sexual contact? Absolutely. I can’t think of an activity that checks all the boxes for monkeypox transmission better than sex. However, I think it is very risky to refer to it as a sexually-transmitted disease. That gives people the impression that sex is the only way monkeypox is transmitted, and that’s not the case.
I should also point out that there is a lot of noise out there suggesting this is just a disease of men who have sex with men. I fear we’re doing to monkeypox what we did to HIV in the early days of the AIDS pandemic. People will point at the fact that over 90% of the cases in the U.S. are men, the majority of whom self report as those who have sex with men, as if that is proof that it is a “gay disease.” There is no such thing. Diseases move through community networks. Trying to claim otherwise only risks putting a stigma on the disease such that others will deny they are infected, maybe even not seek treatment, and put others at risk.
Swann: Monkeypox is not considered a sexually-transmitted infection, although sexual activities between humans can be an efficient way to spread the disease. It can also be transmitted during pregnancy through the placenta, contact through respiratory pathways and by touching surfaces that are contaminated. From previous outbreaks, we also know that transmission can occur when preparing or eating meats from an infected animal, or by being scratched or bitten by an infected animal.
A person can spread it at least from the beginning of symptoms until a rash is fully healed, which can take 2 to 4 weeks. It is not clear how long the virus particles remain contagious on surfaces, although so far direct-to-direct intimate contact has been involved in the vast majority of the cases we know about. Historically, it has been less contagious than diseases we routinely deal with, although the situation could be different in new environments and due to new changes stemming from mutation.
The CDC has a good description online about the ways that monkeypox can be transmitted.
My colleague is right to point out that this has had a big impact on the community of men who have sex with men (MSM), although they are not the only people affected. So far the majority of detected cases have been in that community, and I emphasize “so far.” The initial amplifying events in Europe led to a seeding of the virus in that community and its social networks in the U.S. There has also been a lot of education and focus on testing in that community. It definitely has or can spread to others, such as nurses, maids, prisoners, college students, or commercial sex workers. Transmission may be more likely in congregate living settings, and/or among vulnerable communities with lower access to healthcare. In the Southeast, I am seeing some racial inequities in the reported cases so far, with high rates in Black men. This could be due to a variety of factors. Nationally we have had increased incidence and prevalence of STIs, so there are other communities at risk, partly because the presence of STIs with lesions could make transmission more likely. All of us should be thinking about how to respond to the disease, regardless of whether it is likely to affect us directly.
TA: What can people do to reduce their risk of contracting monkeypox?
Swann: First, if you or someone you know has a known exposure, or if someone has a rash or lesion that is unexpected (especially in the genital area), then get tested. At present, testing capacity has been built out beyond public laboratories to include commercial ones, where the sample is taken by a healthcare provider. If you have a known or suspected case of monkeypox, you may also benefit from treatment, either from a vaccine used as treatment or an antiviral. [Editor’s note: the CDC has a page on monkeypox treatment; the North Carolina Department of Health and Human Service’s (NCDHHS) page on monkeypox testing is here.]
If you don’t have a known exposure but have unexpected rashes or lesions, especially in the genital area, please refrain from intimate activities until you have seen a provider and/or been tested. People with monkeypox should also try to stay away from pets to avoid transmitting it to them. [Editor’s note: you can find the CDC’s list of monkeypox symptoms here.]
In addition, avoid close physical contact with someone who has monkeypox or similar lesions, and avoid touching the objects and materials used by them to the extent possible. Wash your hands often (with soap and water, or alcohol-based sanitizer). Some changes in sexual activity can reduce your risk as well. Since monkeypox is not only a sexually-transmitted infection, condoms may not be sufficient. Risk can be lessened by fewer partners, more skin barriers, fabric cleaning, activities delayed until after vaccination, etc.
If you are at higher risk for monkeypox, you may be eligible for a vaccine. Supplies are limited, and state and local health departments are rolling it out for the highest-risk groups first. Check the guidelines for your local area for locations and priority groups. [Editor’s note: the NCDHHS guidelines for monkeypox vaccination can be found here.]
Koci: All I would add is that there is some speculation that if you received a vaccination against smallpox you might be protected. Specifically, there is some evidence that the smallpox vaccine is around 80% effective against monkeypox. Depending on where in the world you grew up, you may have gotten the smallpox vaccine as a kid. For example, routine use of the vaccine here in the U.S. stopped in 1972, so those who grew up in the U.S. who are 52 or older likely got the vaccine. I would not count on a shot you got over 50 years ago to provide a lot of protection. And again, don’t confuse these with chickenpox. That isn’t going to protect you either. If this outbreak continues, when the vaccine becomes widely available, get it.
TA: I’ve also seen some public-health experts criticizing the government’s response to monkeypox. What’s that all about?
Koci: Monkeypox is way less contagious than COVID-19. We already have FDA-approved vaccines that work against monkeypox. After dealing with COVID-19 for the past 2+ years, testing, tracing and containing monkeypox should be a walk in the park. But it looks like we’re making all the same key early mistakes we made with COVID-19. We’ve been slow to react, and the messaging has been even more muddled.
Swann: I am disappointed with the governmental response so far, although I acknowledge that a full-scale response is difficult when there is already a first pandemic going on. Also, I agree with my colleague about the relative risks related to monkeypox. The initial reports from monkeypox in the U.S. suggest a fatality rate that is lower than that of COVID-19, and it does not spread as easily. COVID-19 remains a significant threat for a large number of hospitalizations, deaths, and long-term health impacts from infections that are likely to occur in the coming months and beyond. Even though monkeypox is less of a risk than COVID-19, we should absolutely take it seriously. It is having a significant impact on individuals who acquire it, and we are at risk of allowing monkeypox to become an ongoing health challenge in the U.S.
There are numerous ways the monkeypox outbreak has identified continued holes in our public health system. At present, states are not required to report cases of monkeypox to the CDC, so we do not have full visibility on the disease. Testing was initially only available in public health laboratories with limited capacity. Even now, the testing positivity is extremely high, suggesting that we have many cases that are going undiagnosed. We did not commit sufficient resources to the newest vaccine for it quickly, so supplies are delayed.
The truth is that our public-health system has ongoing challenges related to responding to a novel virus or new type of disease outbreak. Sustained funding has been a problem for decades, and the structure of our health systems is not optimized for immediate response. We may also have some expectations that are difficult to meet even for private industry. i.e., ramping up from zero to full speed overnight. I prefer to focus on what we can fix immediately and prepare for in the medium term, while learning lessons that we implement for the long-term. This area, too, is changing rapidly, including restructuring of some federal agencies.
TA: How do you think the government’s response to monkeypox was informed by the COVID-19 pandemic? What about the public’s response?
Swann: I can see evidence that the experiences during the COVID-19 pandemic are already starting to inform the monkeypox response. Testing has been expanded to commercial laboratories; the U.S. has procured the largest supply of the new vaccine in the world; the CDC has formed a modeling group and connected with external researchers. We have also seen that some policies have been adapted, as they are rolled out and federal agencies respond to the needs of the public.
As a result of the COVID-19 pandemic, the U.S. public has much greater familiarity with testing, test positivity, transmission in different pathways, etc. We have to be sure that we are clear about the differences, such as the long period of infectiousness of monkeypox, and the relatively lower risk through airborne contact that is not intimate. I think the public also has some fatigue in general about diseases and disasters, with bombardment of other types as well.
Koci: I hate to be more pessimistic, but I don’t really see much evidence that we learned anything from COVID-19. The main problem with our COVID-19 response was how slow it got off the ground from a public health perspective, and how slow the public was to fully appreciate the size and scope of the problem (some still don’t). The sooner you can react the better your chances of being able to control the fire instead of it controlling you. That’s not a new lesson, but one we should have relearned from COVID-19. In January 2020 we watched as COVID-19 spread from country to country. We weren’t doing the amount of testing we should have been, but two days after the first confirmed case in the U.S. the CDC declared a public health emergency. At that point there were just eight confirmed positive cases, but in reality there were likely hundreds, if not thousands, of cases.
Flash forward to 2022. Monkeypox first showed up in Europe in early May, and in a matter of weeks we had the first confirmed case here in the U.S. on May 17th. But it took some 11-12 weeks for the CDC to declare a public health emergency. That was after monkeypox was found in 48 of 50 states, we have over 7,000 confirmed cases, and we account for 30% of all the cases in the world. Just like the early days of COVID-19, public health has had to ration tests, only using them on patients with typical symptoms and known exposures. There have been cases where people and their doctor had to fight to get tested because they didn’t have a known exposure but were confirmed positive. That means there is more community spread than we know about. And just to drive home the point, the CDC has acknowledged that the true number of cases in the U.S. is likely much higher than what we know about.
I’m glad to hear that the CDC is getting people to start modeling spread. And I’m glad that monkeypox was declared a national health emergency. That will make it easier for the CDC and state health agencies to share data. That is absolutely essential if we’re going to have any shot at controlling this better than we are currently controlling COVID-19. But, in my opinion, if we learned anything from COVID-19 it shouldn’t have taken this long to start.
TA: What do you think the public can expect from the monkeypox outbreak in the coming months?
Swann: This could go two ways. In the best case, testing is rolled out widely, vaccines arrive in time, and the number of cases decreases enough so that we could eventually eradicate monkeypox in the U.S. The U.S. would also need to focus on the disease as a worldwide phenomenon, as we have clearly seen that diseases do not know borders. On the other hand, monkeypox could continue spreading undiagnosed in individuals and in communities. In that case, it could become endemic, especially in specific settings like congregate living, colleges, etc., and especially in vulnerable communities that have lower access to healthcare or higher rates of undiagnosed sexually-transmitted infections.
Koci: The next couple of months? With the fact that monkeypox is now in all 50 states, 77% of all cases are men between 18 and 44, and we’re weeks away from the start of the college fall semester, we could see cases really take off. Again the good news is we already have an FDA approved vaccine that demonstrated 85% efficacy against monkeypox. If we can get enough doses of vaccine produced and distributed before the virus is allowed to spread too much more, it is possible that we can control this outbreak.
However, what does this look like over the long-term? Mother Nature has something to say about that too. If we’re lucky, the mutations that made this variant of monkeypox good at spreading in people will mean it no longer infects animals, specifically rodents. If this strain of monkeypox is only a human virus, then we could use the same strategy used in the 1970s and 1980s to eradicate smallpox, and completely control, even eliminate this monkeypox variant.
Given the unbelievable stretch of good luck we’ve all enjoyed since the start of 2020 (is there a sarcasm font?), we may want to develop a hope for the best but plan for the worst strategy. The majority of monkeypox viruses that we know about seem to hang out in rodent species. If this virus can still infect mammals other than people, it will likely find animals in different parts of the world where it can hide – allowing it to jump back into people every so often and in different random places to kick off new outbreaks that we’ll have to incorporate into our new normal.
TA: Do you think we might see cases of monkeypox on college campuses?
Swann: There are some colleges that have had cases, such as Bucknell and Georgetown. Because we do not know the full extent of the spread, we do not know what will happen in the fall semester. There may be some campuses with higher risk than others, such as if the prevalence of monkeypox is higher in their location or if social networks are connected to populations with higher prevalence. I think that campuses should prepare for the potential need to test students. If cases are identified, students may need to isolate for several weeks. I hope that we will not have large numbers of students affected by this, if we deliver a sufficient response in the shorter-term.
[Editor’s note: If you have questions about COVID-19, public health and vaccinations, check out our series of relevant Q&As with NC State experts.]
This post was originally published in NC State News.
- Categories: