Symbiotic strides
Helen Huang and her lab are building better prosthetics by enhancing them with robotics and AI.
On Labor Day in 2013, Greg Phillips left his mother’s house in Somers, New York, to start his 30-minute drive home down the winding country roads the Hudson Valley is known for. While coming around a corner on his motorcycle, he spotted a minivan slowly turning onto the road in front of him. The van’s driver saw him and panicked — instead of hitting the gas, they hit the brake.
“I couldn’t maneuver around them because there were guardrails on either side,” Phillips recalls. “So I went sideways into the car, and it caused a compression fracture. My [right] foot was crushed between the car and the motorcycle.”
After experiencing 22 surgeries, six screws, and a MRSA infection between 2013 and 2015, Phillips decided to have the foot amputated.
“I knew I would be healthier once I could get walking,” he reflects.

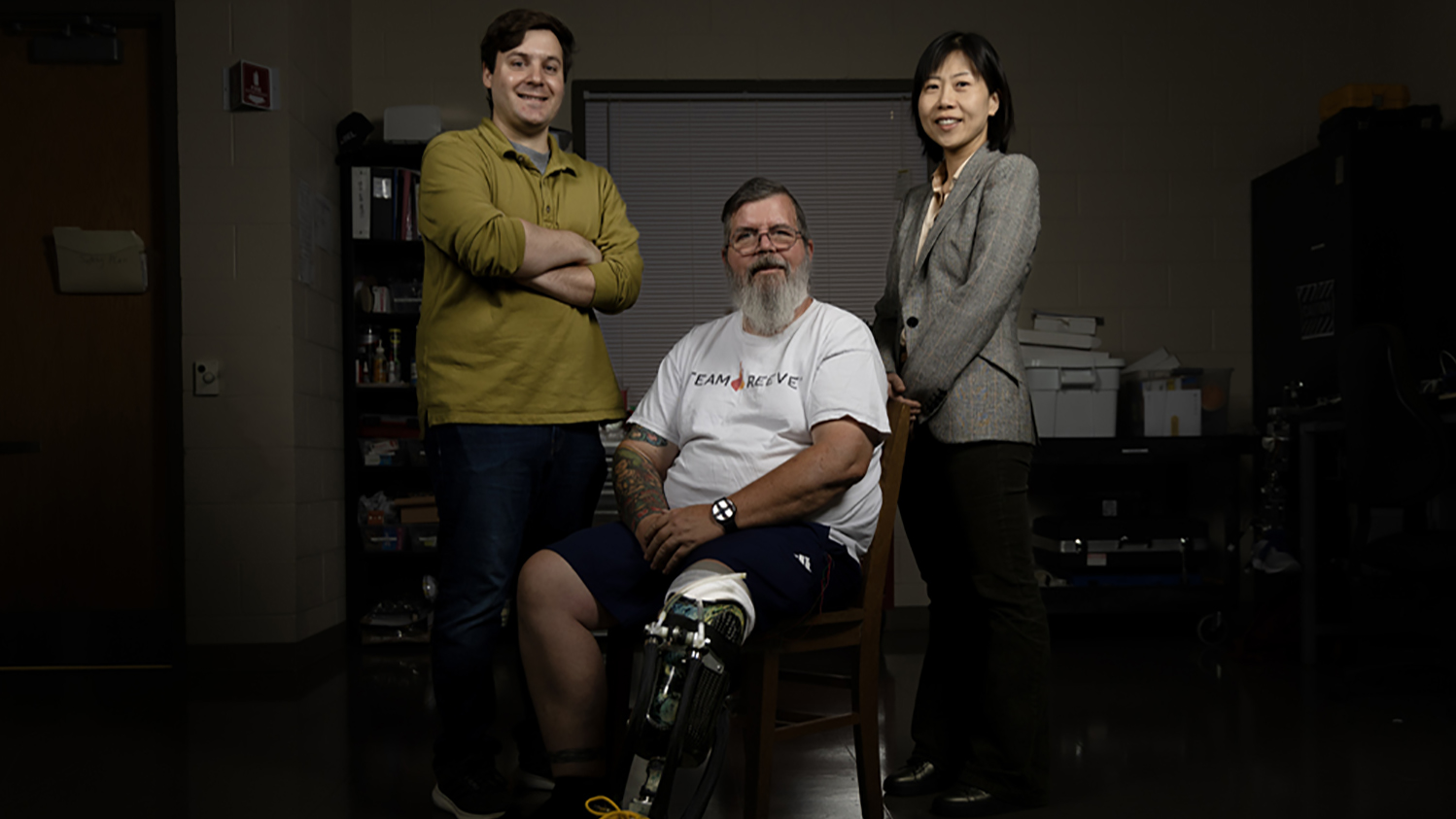
Today, Phillips is a study participant in the lab of He “Helen” Huang, a researcher within the Joint Biomedical Engineering Department — a collaboration between UNC-Chapel Hill and NC State. Huang, who holds full professorships at both universities, runs the Neuromuscular Rehabilitation Engineering Laboratory at NC State, which combines robotics and machine learning with prosthetics to develop next-generation assistive technology.
“Greg has participated in almost every study for lower limb prosthetics,” Huang says. “He’s come to the PhD defense of every student he’s worked with. He’s such a supporter.”
“I’m really blown away by the benevolence of students in this lab,” Phillips adds. “They’re dealing with problems they may never face themselves, but they’re spending their time, efforts, and education to solve them. So if they’re willing to do that, I’m certainly willing to try.”
Huang’s prosthetics connect to existing muscles above an amputation. The remaining nerves activate the muscles, which in turn control the prostheses. The process mimics how the nervous system signals and activates a biological limb.
“The good thing about the human brain is that it is adaptive,” Huang stresses. “It can learn, and if we can train it, we can restore function to these limbs.”
Decoding brain signals
In the late 1990s, when Huang was just an undergraduate student in China, she read an article about researchers who were decoding brain signals in monkeys. Using computers, they could read neural signals from the monkey’s brain to control a computer cursor or robotic arm.
“This was super fascinating to me from a science and engineering point of view,” Huang says.
Huang admits that she was drawn to engineering because she likes math but stayed for the impact it could have on human health — something she got a lot more exposure to during her PhD at Arizona State University. While there, she worked on a project implanting stimulation devices in people with spinal cord injuries, which could help wheelchair-bound individuals stand up and walk.
“I fell in love with working with patients,” she says. “I directly felt the impact of the research.”
Toward the end of her program, she attended a talk by Todd Kuiken, a physician-scientist at Northwestern University who was using a surgical technique that could rewire nerves in the muscles of people who had lost limbs and direct them to control a prosthesis. Then, he brought a study participant on stage to do a live demonstration.
Rather than directly reading brain signals, like the study with monkeys Huang had read about, Kuiken was encouraging the residual nerves to reinnervate muscles — which are biomechanically no longer functional after limb amputations — to power the prosthetic limb. This is a type of neural-machine interface.
Huang went on to pursue postdoctoral training in Kuiken’s lab. Now, one of her research goals focuses on using neural-machine interfaces with upper- and lower-limb amputees.
Building better prosthetics
In the last 20 years, as batteries and mechanical motors have become smaller, lighter, and more powerful, Huang has watched the prosthetics field expand drastically. When she began doing this research in the 2000s, patients were still using 100-year-old technologies. But so much has changed since then.
One difference is materials. Instead of wood and leather, newer devices use plastic, silicone, aluminum, and titanium. Today’s prosthetics are also being combined with 3D printing, motion-sensing technology, robotics, and artificial intelligence — all of which help customize these devices for individual users.

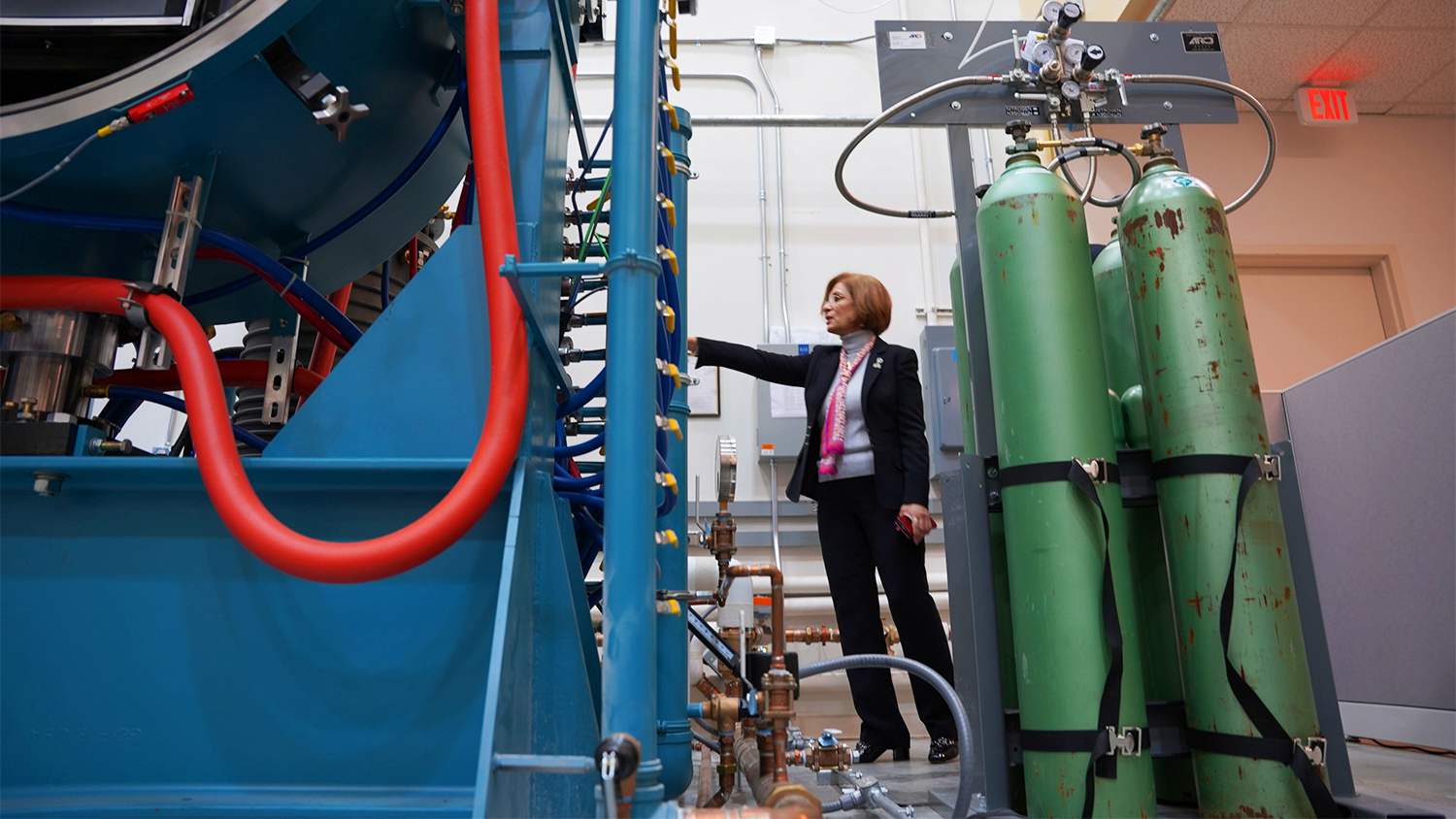
Huang strives to create a symbiotic relationship between humans and these wearable machines. Her students design and fabricate the hardware for the robotic prosthetics and then implement her neural-machine interface to connect with a patient’s muscles and nerves.
To do this successfully, Huang requires all students in her lab to visit the UNC Rehabilitation Center, amputee clinics, and local support groups. This is how they uncover the needs of these patients.
“I was trained in a rehabilitation hospital and that was really helpful,” she says. “You see how the current technology works and learn what patients want.”
Merging expertise
Huang attributes her success to her current and former lab members and collaborators across both UNC-Chapel Hill and NC State. Her team has expertise in mechanical, electrical, and biomedical engineering and even kinesiology, the science of human body movement and function. She also works with physical therapists, medical doctors, and psychologists.
Having a joint department eases the grant application process and saves resources for both schools. Additionally, students in the department can take classes at either school, and their diplomas will list both universities. There’s also a daily shuttle that runs between the two campuses to ease the commute.
“To me, this is a perfect scenario,” Huang says. “Here are two big universities, one with an engineering school and another with a school of medicine. Add them together, and you have a biomedical engineering program that is really wonderful.”
The joint program is one of the largest biomedical engineering departments in the United States. More than half of its faculty have started companies and over 50% of its students go into the biomedical industry in North Carolina.
“The department is very entrepreneurial, with a focus on translating ‘bench to bedside’ to move technologies out of the lab and intro the commercial space to make an impact in patient care,” says Paul Dayton, who chairs the department.
Combining human and artificial intelligence

One challenge for people with lower limb loss is balance. For example, walking up stairs takes both flexibility and power, and uneven surfaces like sand require the ankle to move from front to back and side to side.
Huang’s interface uses electromyographic signals — amplified signals from the remaining nerves that connect to a patient’s residual muscles. It also recognizes the user’s specific movement goals and predicts what their next move might be. In a recent study, this technology improved stability, posture, and body coordination for patients with lower-limb prosthetics.
For upper-limb prosthetics, she’s using machine learning to teach these devices to learn an individual’s movement patterns and translate them into action. Then, an occupational therapist will work with the patient to teach them how to adapt to the device.
“We still have to leverage human brains,” Huang points out. “The machine learning compensates for a portion of the work. We need both intelligences — the humans and the AI — to work together to make the human function better.”
Huang is also developing an exoskeleton that goes over the torso to support walking and balance in people with weak hip joints. It is programmable and offers different modes of assistance or resistance to encourage exercise.
Huang is in the process of creating a startup company for her technologies developed in the lab. In the meantime, she’s collaborating with a commercial prosthetics company so they can incorporate her innovations into their devices for use by people with limb loss in the future.
“I hope to see AI become a bigger portion of our research and rehabilitation clinics. There’s a lot of room to improve these technologies to benefit the patient population and to empower clinicians to perform their jobs in clinics more effectively,” she says. “We have a long way to go.”
He “Helen” Huang is a professor in the Joint Department of Biomedical Engineering at UNC-Chapel Hill and NC State University. She is the Jackson Family Distinguished Professor at NC State and a professor at Carolina. She is also director of the Closed-Loop Engineering for Advanced Rehabilitation core.
Paul Dayton is the chair of and William R. Kenan Jr. Distinguished Professor in the Joint Department of Biomedical Engineering at UNC-Chapel Hill and NC State University. He is also a member of the UNC Lineberger Comprehensive Cancer Center.
This post was originally published in the Joint Department of Biomedical Engineering.
- Categories: